From infrastructural deficit, shortage of staff to ill-equipment, the primary healthcare system in Nigeria continues to remain in a sorry state. This stigma hampers healthcare service delivery in many communities across the country, particularly in remote areas. In this story,
On the 2nd of November 2023, the sun fixed its fiery embrace upon the earth at Maddaci, a remote village in Tambuwal, a local government area of Sokoto State. Two children, one about three years and the other eight years old, sat inside a room, grappling with smoke while looking after the food their mother put on fire.
Devoid of windows and ceilings, part of the house’s roofing is left open for the sun to peep into. It looks dilapidated and tattered, with no doors and some of its walls collapsing—nothing close to a dwelling place.
Unfortunately, that place is the staff quarters of Maddaci Primary Health Clinic, where Alhaji Adamu, a man in his early 50s, stays.
“This is where I have been staying with my family for the past nine years,” Alhaji Adamu told this reporter.
Beside the house, is a similar building, and in the front, the facility is situated—all entrenched in a shrinking fence.
As of last November, a community health extension worker, Alhaji Adamu, has been transferred to another facility but has yet to do a handover. He said he had been the only staff working in the facility for the past nine years, adding that if the government assigned workers to the PHC, they would rather shrug off the assignment.
“They will only sit in their comfort zones and collect the salary. One of the primary reasons for this is because there are no staff quarters to accommodate them. You don’t expect all people to come and stay in these buildings just like me.”
Alhaji Adamu is a native of Tambuwal, a town over 40 kilometres away from Maddaci. Marked with horrible potholes, the road from Tambuwal to Maddaci is not motorable after passing Romo, the last village linking Maddaci.
Most of the staff assigned to the facility, Alhaji Adamu said, are from Tambuwal or even far away, and the absence of accommodation and basic amenities left many to either process redeployment or sit back and collect salary without working.
A public health expert, Mr. Tolulope Oni described this act as the “attitude of community health workers,” stemming from the absence of basic social amenities like telecommunication networks, electricity in the remote areas of the country.
“A government will post a community health worker to a particular place, but the person would decline going there because it’s too far,” he said. “And also because there are no basic amenities in the area.
“Meanwhile, it’s also the fault of the health workers because they are mandated to work with the communities directly.”
Mr. Oni said the government needs to take upon itself to fix amenities.“I feel like this measure would have a reverberating effect. When I say a reverberating effect, it means that when one of these challenges is being solved, naturally, it’s going to eradicate some of the other challenges.”
“For example, having full Internet access, electricity among others. I bet most of the health workers would even prefer to live in the villages than in the cities because the cost of living is quite cheap there.”
Madacci Health Clinic Fails to Meet Minimum Standards
The facility itself is nothing to write home about. Started in 2007, it is registered on the website of the Federal Ministry of Health as a functional facility. However, the structure looks nothing but abandoned when this reporter visited it in November 2023.
The doors and bed frames in the ward were broken, mattresses lay tattered, and the entire premises was littered with a leaky roof, broken ceilings and cracked walls.
To wit, the Primary Health Centre (PHC) facility completely falls short of the minimum standard recommended by the National Primary Health Care Development Agency (NPHCDA).
According to the NPHCDA, there is an inadequate number and proportion of the various cadres of healthcare workers necessary to provide services in the health facilities. The agency, in the publication titled; “Minimum Standards for Primary Health Care in Nigeria,” says an ideal primary health care facility should have a minimum of 24 staff.
It recommends that a standard PHC should have one medical officer “if available”; one community health officer (CHO); four nurses or midwives; three CHEW; one pharmacy technician; six JCHEW; one environmental officer; one medical records officer; and one laboratory technician.
For supporting staff, NPHCDA states that PHCs should have two health attendants, two security personnel and one general maintenance staff.
Apart from personnel, NPHCDA also recommends that PHCs should have a well-equipped open ward, labour room, children and female wards, doctor’s office and staff quarters, an ambulance for referrals and drugs and equipment for immunization, preventive and basic curative care.
“All the equipment is worn out. We don’t have any source of water.”
“The facility needs a serious renovation because all the rooms are leaking, even inside my consulting room,” Alhaji Adamu said.
One of the residents who identified himself as Yunusa, said he had to send for all the drugs prescribed for his treatment elsewhere.
This reporter met Yunusa suffering from a serious laceration on his hand at the premises of the facility, waiting for Alhaji Adamu to attend to him. Both Yunusa and Alhaji Adamu bemoaned the lack of equipment and functionality of the PHC.
“I had to go and buy all the drugs prescribed for my treatment elsewhere. We are calling for our aid over this facility,”Yunusa said.
Sadly, about six years after the immediate past president Muhammadu Buhari flagged off a scheme to revitalize over 10,000 PHCs across Nigeria, only less than 25 percent of primary healthcare facilities are functioning.
The Federal Government kicked off the PHC revitalization Programme in January 2017, under which it committed to revitalizing 10,000 PHCs across the country with at least one center in each of Nigeria’s 109 senatorial districts.
Yet, about 80 percent of facilities in Nigeria are still non-functional. The report revealed that there are 34,076 PHCs in Nigeria, accounting for 85.3 percent of total hospitals and clinics in the country. Of this number, it is estimated that only 20 per cent are functional.
“Most of the PHCs cannot provide essential healthcare services, in addition to challenges of poor staffing, inadequate equipment, poor condition of infrastructure, and a lack of essential drug supply,” the report further revealed.
In the same vein, the World Health Organization (WHO) reported that only a quarter of PHCs in Nigeria have more than 25 percent of the minimum required equipment package, adding that “the capacity to provide basic emergency obstetrics services is limited to about 20 percent of the PHC facilities.
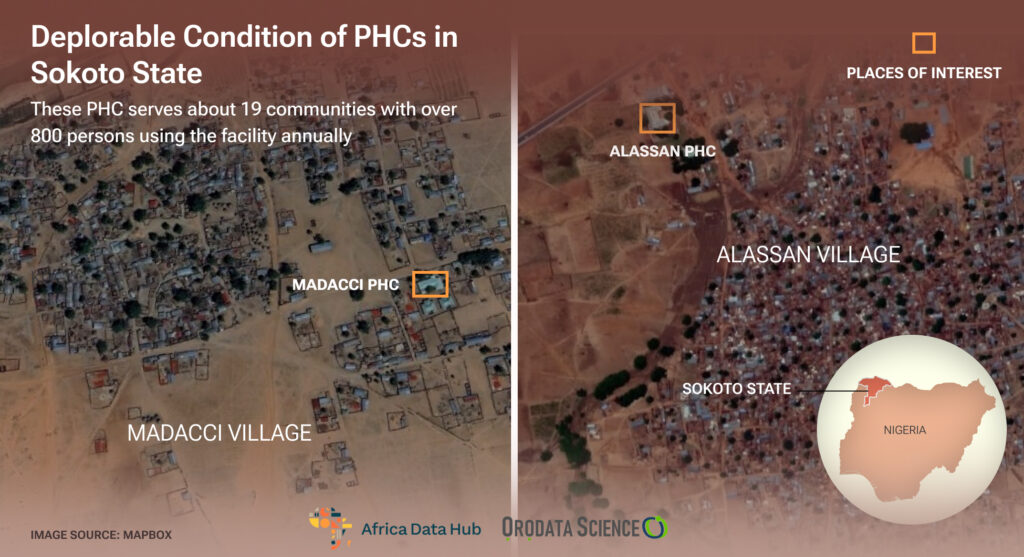
In Alasan PHC, Patients Use Mats as Hospital Beds
The Maddaci PHC is not the only facility that has fallen victim to the government’s negligence. When this reporter visited Alassan Primary Health Center in November 2023, the facility was a replica of Maddaci PHC regarding ill-equipment and infrastructural deficit.
The roof, defeated by the heavy burden of neglect and raindrops, looked bereft of extended maintenance.
The windows are cracked and stained; dust motes hovered in the air. The hospital beds looked abandoned with no sofas; the ones with sofas are tattered and covered by dust, while ceilings remain broken and dangling.
The hospital beds’ sorry state and scarcity make most patients bring along their mats.
“We used to bring our mats along whenever we had patients because we already knew that there were not enough hospital beds,” Dan Gada, a resident of Alassan, said.
Also, in an interview with one of the staff who craves anonymity, he said he spends N1,000 every day on transport because there are no staff quarters.
“I used to come from Tambuwal and I buy fuel for my motorcycle N1,000 every day because there are no staff quarters to accommodate me.”
The lack of an ambulance also poses a grave challenge to the facility. According to the staff, “Whenever we have a case of referral, we arrange with relatives of the patient to convey the person to the designated hospital.”
Underfunding
The founder and chief executive officer of The Health City, Dr. Odunola Olabinta identified underfunding as a stumbling block to the effectiveness of PHCs in the country.
“A lot of these PHCs are underfunded,” she said. “The budget for PHCs in the country is meagre, and what’s even getting to the PHCs themselves is worse.”
Amidst the poor performance of the health systems, the African heads of state and government under the African Union (AU) committed in April 2001 to dedicate at least 15 percent of their annual budgets to the health sector — now known as the ‘Abuja Declaration.’
However, a review of the Nigerian budgetary allocation to the health sector in the last 21 years showed that the country has never met the 15 per cent target agreed upon in the Abuja Declaration.
In 2023, Nigeria allocated over N1 trillion to the health sector for the first time in its funding history. The amount represented about 5.75 per cent of the total budget for the year.
Although the Nigerian 2023 budget shows a significant increase from the N826.9 billion allocated to the health sector in 2022 and the N547 billion allocated in 2021, it still needs to meet the commitment made by African leaders under the Abuja Declaration.
Dr. Odunola said there’s also a problem with leadership. “There’s no competent leadership, and once leadership is bad, there would be mismanagement of resources.”
“From misappropriation of funds to inadequate staff and facilities, the problems are myriad coming from the aspect of human resources, the aspect of government to the aspect of leadership.”
She said PHCs need to be heavily funded because when 25 percent of them work in the country, it means there’s a big problem.
“There has to be proper monitoring and evaluation and proper training of staff. So that they will know how to manage resources and facilities that are out there.”
“Whether we like it or not, we have to make PHCs work. Because we can not continue to rely heavily on tertiary and secondary institutions, those institutions, too, are underfunded, and they don’t have enough facilities.”
“So, if the PHC system works, it takes the burden off the secondary and tertiary hospitals, and you know PHCs are closer to the people. The fundamental idea of the PHCs system is fantastic, just that the way we deliver it is not okay. For us to have a good health care system in Nigeria, PHCs have to work.”
Sokoto PHCDA Keep Mums
As of the time of filing this report, the Executive Secretary of the Sokoto State Primary Health Care Development Agency(PHCDA), Dr. Larai Aliyu has not responded to questions posed to her.
The only reply she gave through WhatsApp was: “I shall consult my directors who were here earlier than me and articulate my explanations for your perusal.”
However, further reminders were sent to her, including a letter requested before granting further interview, but have not been responded to.
Meanwhile, in an interview with the Sokoto State Director Public Health, Dr. Abdulrahman said the state’s PHCDA is the best quarters to respond to the questions.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science.