Cross River State’s primary healthcare system, a vital component of its healthcare infrastructure, is grappling with significant challenges despite increased investments by the state government. In recent years, the government has allocated substantial funds to the healthcare sector, with a total of N12.8 billion budgeted for healthcare in 2022, representing a 20% increase from the previous year. However, this figure ranks as the ninth-lowest healthcare budget among all 36 states, highlighting a need for more substantial investments.
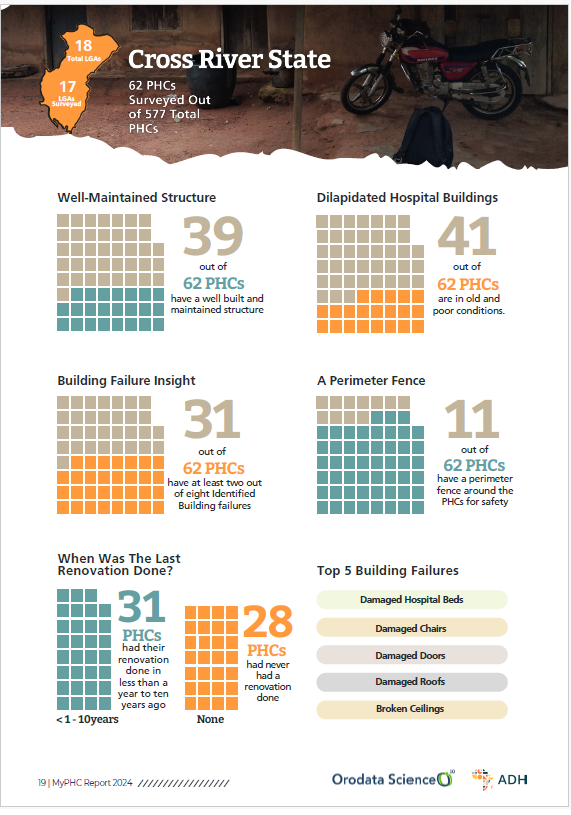
Research data reveals that out of 62 Primary Healthcare Centers (PHCs) in the state, only 31 have undergone renovation in the past decade, leaving 28 facilities in a state of disrepair. Alarmingly, half of these PHCs are struggling with two out of eight identified building failures, compromising the safety and effectiveness of healthcare delivery and putting both beneficiaries and healthcare providers at risk.
The state government’s investment in healthcare rises annually, but the data highlights a significant need for targeted infrastructural upgrades to ensure safe and effective healthcare delivery. To maximize the impact of its investments, Cross River State must prioritize renovation and maintenance of its PHCs, focusing on the 28 dilapidated facilities and addressing the identified building failures. By doing so, the state can strengthen its primary healthcare system, ultimately enhancing the health of residents.
Infrastructure and facility challenges persist, with 42 out of 62 PHCs lacking clean restrooms and relying on unsafe waste disposal methods. The inconsistent power supply, often courtesy of solar panels, underscores critical gaps in basic infrastructure, posing grave health and operational risks to patients and staff alike.
The scarcity of vital medical equipment and supplies across the state’s PHCs is alarming. A mere two facilities possess functional ambulances, whilst only 28 boast pharmacies. Moreover, chronic shortages of essential items such as oxygen and personal protective equipment (PPE) critically undermine emergency response capabilities and overall healthcare delivery, leaving patients vulnerable to suboptimal care.
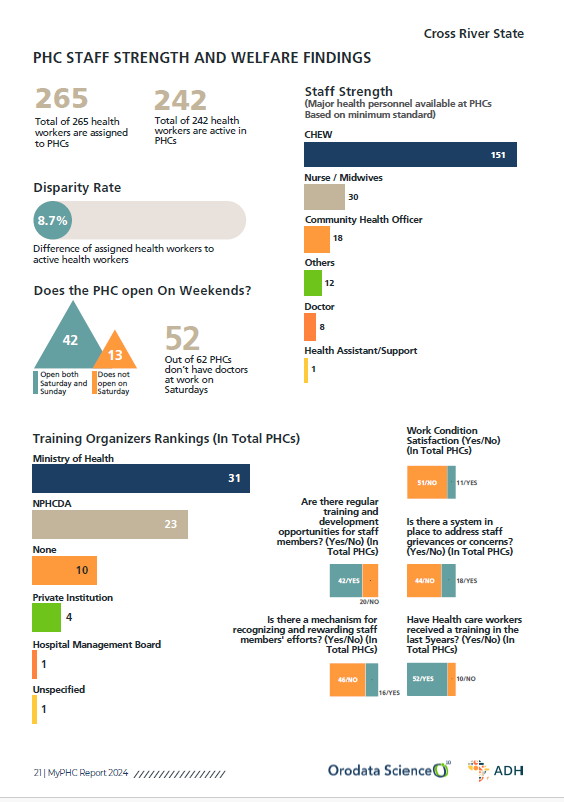
Staffing challenges also plague the state’s PHCs, with a notable discrepancy existing between the assigned and active health workers. The majority of facilities lack medical doctors during weekends, disrupting continuous healthcare services and highlighting a need for more effective workforce planning.
Weekend service provision and staffing in Cross River are also concerns, with 13 facilities remaining closed and impacting access to healthcare. The staffing composition includes 151 Community Health Extension Workers (CHEWs), 30 Nurses/Midwives, and a mere 8 Doctors, among others. However, a concerning 40 out of 51 PHCs report dissatisfaction with work conditions, underscoring the need for improved staff morale and a more conducive work environment.
Staff support and development in Cross River are inadequate, with only 18 and 16 PHCs respectively having formal mechanisms for addressing staff grievances and recognizing their efforts. Although 42 facilities offer regular training, and 52 have provided training in the last five years, primarily facilitated by the Ministry of Health and NPHCDA, there is a need for more comprehensive support structures to enhance staff development and motivation.
Patient utilisation and community engagement in Cross River are affected by financial barriers, with a concerning 41% of patients struggling with affordability. Referral patterns and reasons highlight critical gaps in PHC capabilities, with 694 referrals recorded over the past year primarily due to complications, prolonged labour, and infrastructure inadequacies.
Treatment quality and service ratings in Cross River vary significantly, with 32 PHCs’ treatment quality rated as excellent or good, and 17 rated poor or very poor. Immunisation services fared better, with 50 PHCs rating excellent or good, and 12 rating poor or very poor. Overall, 34 PHCs received excellent or good general ratings, whereas 28 received fair or very poor ratings.
For a more detailed analysis and recommendations, download the report. [Click here]