“Sometimes, we work with only hope and prayers,” murmured a Nurse who wished to by anonymous*, her voice nearly drowned by the hum of a faulty ceiling fan. In one of the center’s dusty wards sits a rusted metal bed, covered with a threadbare mattress and soiled fabric, surrounded by scattered debris and exposed electrical cables. It’s not the aftermath of a renovation — it’s the current state of care.
A rusted hospital bed with torn mattresses and makeshift coverings at Atoruru Primary Health Center. Exposed wires and debris litter the floor — a scene that reflects the facility’s deep state of neglect.

(Photo: Osaiyekemwen Confidence Osarumwense)
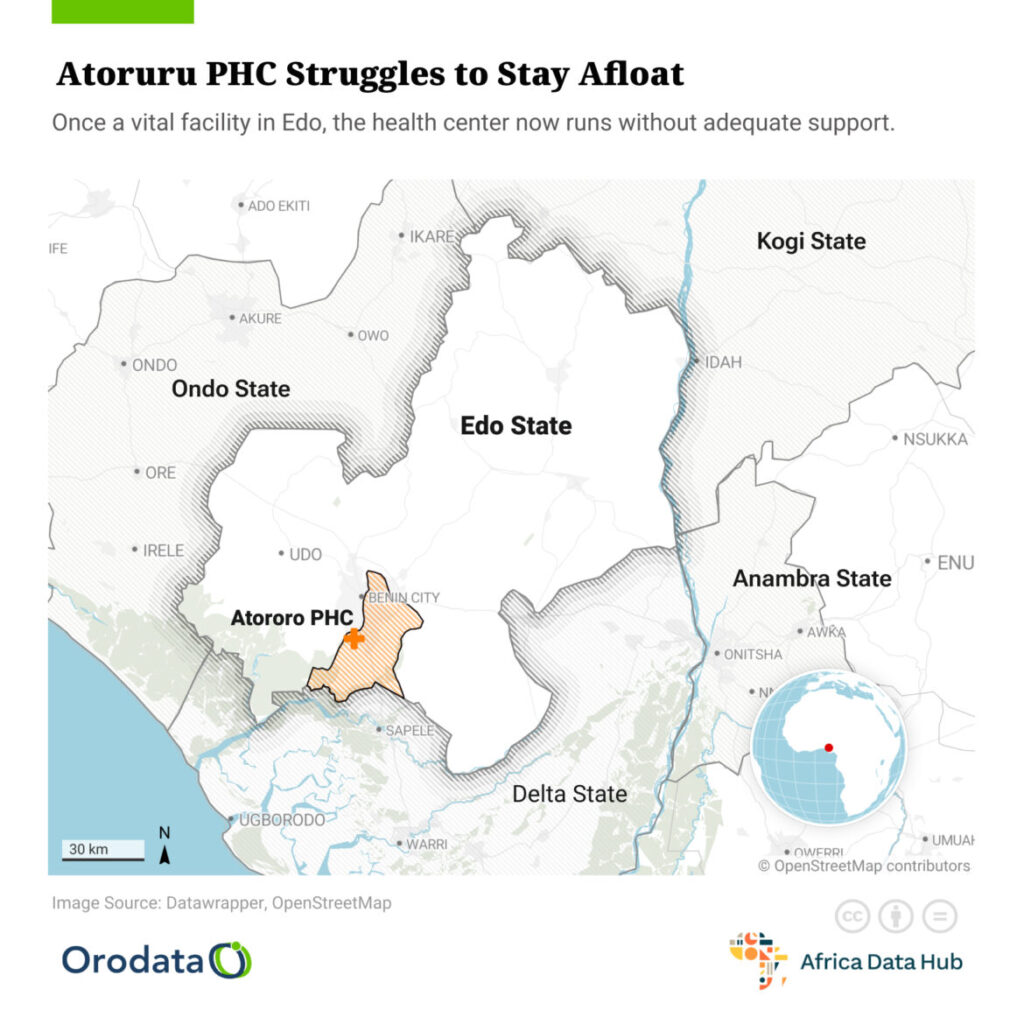
Nestled in the heart of a densely populated community in Edo State, Atoruru Primary Health Center was once a beacon of hope — the first point of contact for many seeking affordable healthcare. Serving thousands of residents, including children, pregnant women, and the elderly, it was meant to be a lifeline. Today, however, it stands on the brink of collapse. With inadequate staff, crumbling infrastructure, and severe shortages of drugs and medical supplies, the facility now mirrors a neglected outpost rather than a place of healing.
This report investigates how a once-promising healthcare facility has slipped into crisis — and what it means for the people who still depend on it for survival.
2. The Current State of Atoruru PHC
Walking through Atoruru Primary Health Center feels like stepping into a forgotten space — one where healthcare is attempted against all odds. The walls are stained, beds are either broken or overcrowded, and vital equipment is obsolete or entirely absent. In some wards, the smell of damp fabric and disinfectant barely masks the odor of neglect.
The center is supposed to cater to a population of over 10,000 people, yet it struggles to maintain even the most basic services. There is no functioning laboratory. The delivery room lacks proper lighting. Critical supplies such as gloves, antiseptics, and even clean water are scarce. Patients often arrive with hope but leave with referrals to private clinics they can’t afford — or with untreated conditions.
Staff members are stretched thin. A single nurse may manage an entire ward during a 12-hour shift. “We do more paperwork than care work because we have no tools to actually treat patients,” one health worker lamented. “We improvise — sometimes dangerously — just to keep people alive.”
The building itself is crumbling. Ceilings leak when it rains, and some rooms are unusable due to flooding or mold.

” Source: CheckMyPhc, Orodata & Africa Data Hub). This visual comparison highlights how Atoruru PHC’s issues reflect a wider pattern of infrastructural decay in Edo State’s primary health care system.”
Sagging, water-stained ceilings at Atoruru Primary Health Center pose a daily threat to patients and staff. The facility’s deteriorating infrastructure has become a symbol of chronic neglect.

(Photo: Osaiyekemwen Confidence Osarumwense)
Despite these glaring problems, the facility has not received any meaningful upgrades or government support in years.
Atoruru PHC is not just underfunded; it is abandoned in slow motion.
3. Voices from Within
Behind the peeling walls of Atoruru PHC are the stories of healthcare workers who carry the weight of the crisis daily — often in silence, often unnoticed.
“We come to work knowing we may not have what we need to save a life,” said a nurse who has served at the center for over eight years. She asked not to be named, fearing repercussions. “We beg patients to buy their own gloves and syringes. Sometimes, they can’t, and we watch them deteriorate.”
Another health worker described the emotional toll: “It’s not just the tools we lack — it’s motivation. We are tired, short of equipment, and forgotten.”
Patients are no less vocal. A young mother who brought her child for treatment shared her ordeal: “They told me to go buy paracetamol and bandages outside. How can a PHC not have common paracetamol?” Her frustration echoes through the waiting area, where many sit on broken benches, fanning themselves against the oppressive heat.
Even junior staff are affected. Cleaners and clerks lament delays in wages and unsafe working conditions. One cleaner pointed at the broken ceiling with visible fear: “We pray every day it doesn’t fall on someone’s head.”
4. Accountability and Governance
The crumbling walls of Atoruru Primary Health Center are not just signs of physical neglect; they are symptoms of a broader failure of governance.
According to local health policy guidelines, primary health centers like Atoruru are the backbone of Nigeria’s grassroots healthcare delivery system. They fall under the purview of the Local Government Health Authority (LGHA) in collaboration with the Edo State Primary Health Care Development Agency (EDSPHCDA). Yet, despite this multilayered oversight structure, Atoruru PHC remains starved of funds, staff, and basic support.
Community members report that politicians often visit the facility during election campaigns, promising renovations and upgrades. “They always say, ‘We will fix this place,’ but after elections, they vanish,” said a local youth leader, frustrated by years of broken promises.
A review of Edo State’s health budget allocations from the past three years reveals significant discrepancies. While funds are reportedly earmarked for PHC revitalization, frontline facilities like Atoruru see little or none of it. Transparency is further clouded by the absence of public records detailing how local councils disburse or utilize these funds.
Civil society groups and advocacy platforms like Nigeria Health Watch and TrackaNG have raised alarms over the neglect of rural health centers across the country. In 2023, a report by one such group listed Atoruru among 15 “red flag” facilities needing urgent intervention in Edo State. Still, no official action has followed.
“Accountability mechanisms are weak or non-existent,” said a health policy analyst based in Benin City. “There’s no reliable feedback system for community members to hold local health officials accountable. Most people don’t even know who to report to.”
As it stands, Atoruru PHC continues to function on autopilot — propped up by the sheer will of overburdened staff and the desperation of a community with nowhere else to go.

Without deliberate intervention — from both government and stakeholders — the center may soon collapse entirely, leaving thousands without access to even the most basic care.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science.